From the author: This article originally posted in early December 2020 with the title, “I will get a COVID-19 vaccine.” I feel fortunate to have finished my two-dose sequence in late February and received a booster when I became eligible.
Vaccines have been and continue to be widely available to EMTs, paramedics, firefighters, corrections officers and police officers. If you are vaccinated, thank you! If you are unvaccinated, please consider getting vaccinated for your own safety, as well as the health and safety of your family, friends and coworkers. If you are a public safety employer, offer incentives, prizes and paid time off to encourage vaccination in your remaining unvaccinated personnel.
As soon as a COVID-19 vaccine is offered to me, I will say “yes, please.” Even though as a relatively healthy non-clinician, I might be in the middle or even near the end of the line, I am counting the days until I bare my deltoid and watch a dose of freedom and return to normalcy plunge into my muscle. You can be sure I will show up for the second dose.
If you are an active EMS provider, in the CDC group 1A, I hope you are eagerly planning to receive a vaccine as soon as its available to you. Just as importantly, I hope your EMS employer is aggressively advocating for you and your colleagues to be among the first to receive vaccination in your state, as well as to help administer the vaccine to skilled nursing facility staff and residents, to corrections officers and inmates and through clinics for other relatively high-risk groups like firefighters, police officers and senior citizens.
4 ‘Ps’ of Scene Size-up
As a Wilderness Medical Associates instructor, I taught wilderness first aid and first responder students to use the 4 Ps mnemonic before initiating patient care. The Ps stand for:
-
Provider
-
Partner
-
Public
-
Patient
Provider safety is #1
Provider means assessing the risks to yourself. There is an endless list of threats and dangers to EMS providers during patient assessment, treatment and transport. The risk of COVID-19 infection, on- and off-duty, is significant. Dozens of EMS providers have died from COVID-19, and tens of thousands have been exposed, with some becoming severely ill. The risk of COVID-19 death for paramedics is greater than for nurses, physicians, firefighters and police officers.
Standard PPE precautions – gloves, mask, gown and eye protection – are not enough to ensure provider safety. Social distancing is impractical to impossible on the job. The CDC recognizes the inherent risks of out-of-hospital patient care and has assigned EMS to the first group of vaccine recipients.
The “COVID-19 Vaccination Considerations for Paramedics,” released Dec. 7, from the American Paramedic Association and National EMS Management Association states:
“Paramedics are not being placed at the head of the vaccination line as ‘guinea pigs.’ Instead, the CDC and Federal officials have finally recognized our significant contribution to treating and limiting the spread of this disease and are protecting us accordingly. This is an opportunity we should not squander.”
A significant impact of the pandemic on paramedics has been constant and significant stress.
“A COVID-19 vaccine would provide another means to protect EMS providers physically and provide some psychological relief from this harmful virus,” Maria Beermann-Foat, PhD, MBA, NRP, battalion chief of operations for MED-ACT- Emergency Medical Services wrote. “Since the chances of becoming infected increase with more frequent or longer contact times with infected patients, frontline workers would likely experience less stress and greater confidence in being protected from the virus. Vaccination provides a biological level of protection that is not compromised by possible human error each time a COVID-19 patient is encountered.”
Vaccination also confers off-duty benefits for paramedics. EMS1 regularly receives news items and anecdotal reports that paramedics and other public safety providers don’t practice adequate infection prevention control off-duty. All paramedics, to minimize provider risk, need to diligently wear a mask, practice social distancing, minimize exposure to anyone who may be symptomatic or asymptomatic and regularly wash their hands. Vaccination is especially critical for those among us not following infection control guidelines off duty.
Vaccinate for your public safety brothers and sisters
During the scene size-up, assess for risks to your partner. Some risks may be obvious, like a still running vehicle after a collision. Other risks are hidden from view, like hepatitis, coronavirus or other potential infectious material. Once risks are identified, attempt to mitigate the risk – turn off the vehicle, block traffic from the scene, call the police and don PPE, if not already completed.
Vaccination is a risk mitigation technique we take to protect ourselves from the patient and protect our partner and the patient from us. In a disappointing survey, about 55% of respondents to a FDNY Uniformed Firefighters Association poll answered “No” to the question, “Will you get the COVID-19 Vaccine from Pfizer when the Department makes it available?”
The FDNY UFA survey is not surprising because only one-quarter of respondents to an EMS1 COVID-19 vaccine survey answered “Yes” to the question, “When an approved COVID-19 vaccine is available in the U.S., will you be vaccinated?” Forty-one percent of the respondents selected “No,” 19% opted for “Unsure” and 12% chose “Only if mandated by my employer.”
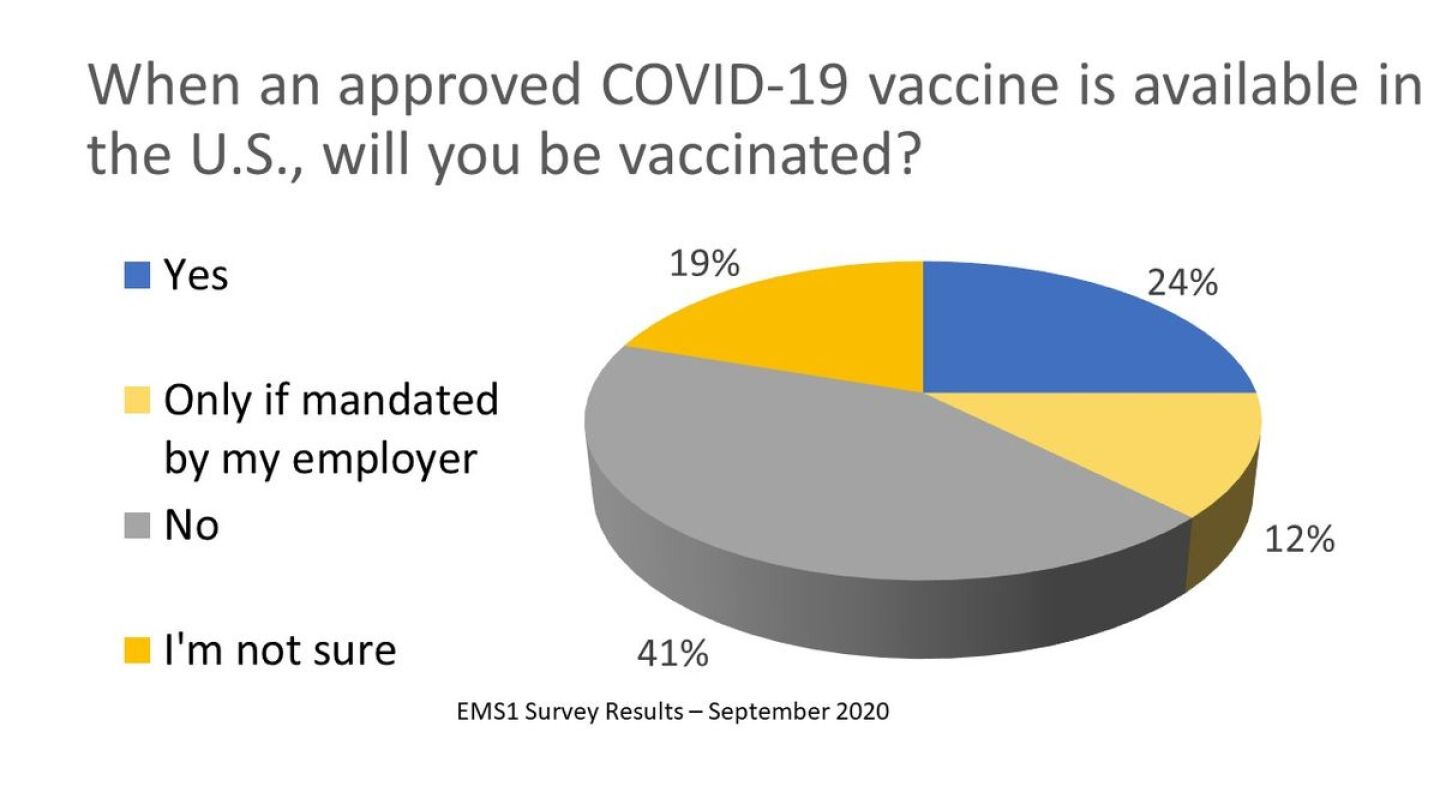
Photo/EMS1: Will EMS providers get vaccinated from COVID-19?
Vaccination is a risk mitigation strategy to improve scene safety for you (the provider) and your partner. Opting out of vaccination is not dissimilar to driving the ambulance too fast for conditions, leaving an exposed needle on the squad bench, or reversing the ambulance or apparatus without a spotter. As you make a vaccination choice, consider the benefit it confers to your public safety brethren as it is disheartening that I might be able to get a vaccine sooner rather than later because 50% or more of paramedics, firefighters and police officers might choose not to get vaccinated.
In the 4 Ps in the scene size-up, the public is not limited to the patient’s family or friends, or other gawkers that are part of every patient contact. Consider a more inclusive definition for the public when evaluating the scene for risks, including COVID-19 and other infectious diseases. The APA/NEMSMA document includes this important reminder:
“Among all public health and safety professions, paramedics are the only ones that routinely contact all of the other first responders and essential healthcare workers. In every shift, paramedics encounter hospital staff, law enforcement officers, firefighters, long-term care facility residents and staff, and the general public.”
Your circle of friends or pandemic bubble overlaps with lots of other circles and bubbles. Missing, but perhaps most important, in the inclusion of the public is your immediate family or roommates – the people you return to after each shift.
Throughout the pandemic, the greatest fear of any paramedic is bringing COVID home. Many paramedics have adopted elaborate post-shift procedures to undress in the garage, launder uniforms and shower before greeting their spouse, significant other or children. Vaccination trumps all of those techniques in reducing risk of harm to the broadly defined public paramedics encounter on- and off-duty.
Patient comes last
The scene size-up, like the primary assessment, isn’t a discrete evaluation of risk to provider (self) then partner then public, but rather a simultaneous evaluation of risks as they are identified and mitigation with the tools and training available to you. Nonetheless, vaccination, though the ethical thing to do, is least important for the patient. The patient is already ill or injured and the likely beneficiary of your PPE, sterile techniques and disinfection practices.
We also ought to consider patient more broadly than the currently ill or injured. Everyone in your service area is a potential patient for trauma, sudden cardiac arrest or COVID-19 infection. Paramedics, EMS leaders, other public safety professionals and all healthcare providers play a critical role in illness and injury prevention. This role includes educating the public about vaccination, role modeling the willingness to participate in risk mitigation efforts and participating in COVID-19 vaccination distribution and clinics.
Vaccination protects against the worst-case scenario
When I use PPE, vaccination and other infection control practices to prevent hepatitis infection, I am not motivated to do so because of worry about experiencing a mild case of hepatitis. Instead, I am motivated by worry about the worst-case of hepatitis, leading to liver failure, interminable waiting on a transport list and eventual early death.
Similarly, for COVID-19, my worry isn’t that you, your partner, your family or your patient experience asymptomatic COVID-19 or a mild case. Instead, my worry is standing by helplessly and remotely as someone I care about clings to life on a mechanical ventilator. I don’t want any of you, anyone I know or anyone I love to have their breathing supported by a machine alone in a hospital room.
My fear of the significant, known risk of severe COVID-19 infection is much greater than the extremely low probability of adverse response to a vaccine. Emergency, Army and SWAT physician Jason Pickett, MD, put it this way in a Tweet:
“Will I get a COVID vaccine? Emphatically yes. I haven’t gotten to review the safety data on them, but for the past year I have been reviewing the safety data on the virus itself, and it’s abysmal. With so many poor outcomes from the virus, I’ll take my chances with a vaccine.”
Finally, if you opt-out of vaccination during Phase 1A, it might be difficult to get back in line as some immunization experts “expect attitudes to shift quickly from widespread hesitancy to urgent, even heated demand.”
I will be at the back of the line with my friends and colleagues Hilary Gates, EMS World senior editorial and program director, and AJ Heightman, editor emeritus of JEMS, cheering for as many paramedics, healthcare professionals and other public safety professionals to be millions of places ahead of us. Please #GetVaccinated.
Read Hilary’s #EMSVax editorial on EMSWorld.com and AJ’s encouragement to take the vaccine on JEMS.com



